Digging into the Carbohydrate-Insulin Model of Obesity

Read time: 6 min
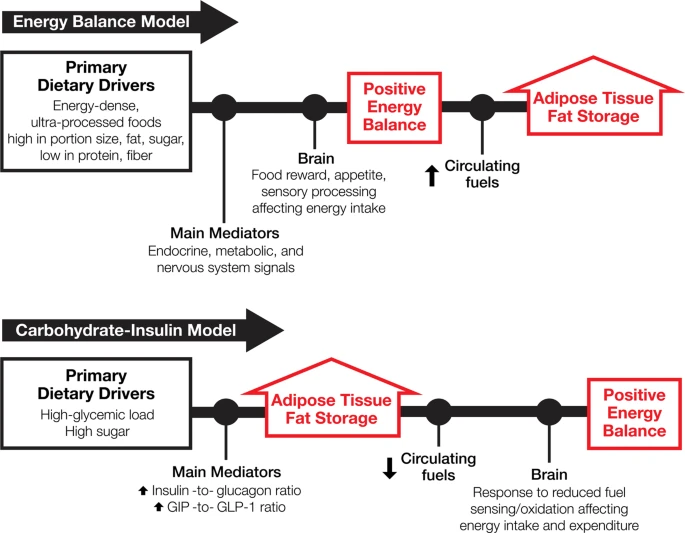
Dr. Ludwig never disappoints! He and his team released a paper in the #European Journal of Clinical Nutrition contrasting the prevalent theories regarding obesity (what most people call the Energy Balance Model or EBM) with the newer model that is being thrown around (the Carbohydrate-Insulin Model or CIM). Despite pushback from peers and patients and everyone in between, I have been teaching the CIM for years. The science is simply too good to ignore.
Not to mention the fact that the EBM is built upon the foundation that the accumulation of excess weight is a personal responsibility issue that must be solved by forcing people to endure misery to atone for the moral failings that led to the accumulation of unnecessary weight. And then, to add insult to injury, pulling that blame back around a second time when they can’t endure the misery of treatment.
Having spent my career taking care of thousands of people with obesity, I can say with complete certainty that moral superiority or strength of character is definitely not something that separates people with obesity from those without.
Embracing the carbohydrate-insulin model of weight accumulation takes a little extra thought – relying on biochemistry and physiology instead of simple mathematics – but it’s not exceptionally complicated or difficult to understand.
Dr. Lugwig and his team say it this way, “a high-glycemic load (GL) diet—one with large amounts of rapidly digestible carbohydrates (i.e., free sugar, processed grains, most starchy vegetables)—elicits hormonal responses that inhibit fat mobilization (lipolysis) and promote fat deposition in adipose tissue. As recently detailed, consumption of a high-GL meal … shifts substrate partitioning toward deposition, leaving less energy available. The brain responds by activating pathways controlling hunger and other appetitive responses to promote energy intake. If an individual resists the drive to eat by restricting food, metabolic fuels are conserved through reduced energy expenditure manifesting as fatigue (leading to sedentary behavior), decreased non-exercise activity thermogenesis, increased muscular efficiency, and other mechanisms.”
I explain it to my patients like this (it’s a little less scientific but easier to comprehend), “when you eat a diet consisting of a lot of foods that your body isn’t designed to metabolize (sugar and simple carbohydrates), it goes into panic mode and does its best to get those things out of circulation and stored away, which it does in the fat stores. However, the hormones released as part of that storage process essentially lock up those fat stores, so when the body needs fuel again, it can’t access it, so the brain has to ask for more. The repeat administration of these same foods begins the process all over again – consume, store away, need, ask for more, consume, store away, need, ask for more – over and over again. This constant cycle creates two things – dysfunctional thinking about food and a decreased responsiveness to the hormones, which drives hormone resistance and an overall worsening of the problem. Both of these subsequent problems make treating the original problem much more difficult.”
The CIM also helps explain the marked heterogeneity in response to macronutrient-focused weight loss diets. In other words, perhaps some bodies respond more vigorously to a high glycemic-load diet than others – just like some respond more vigorously to medications or vaccines, or environmental toxins. We’ve all known people that eat a terrible diet their entire lives and never accumulate excess weight. Perhaps, rather than congratulating these individuals for being able to perfectly balance their calories year after year (thereby assuming they have a more robust strength of character and/or discipline, which is what the EBM assumes), we should chalk them up to having a better genetic resiliency to the food – just like those people that can smoke cigarettes their entire lives and never develop lung disease.
We still have work to do to shift the treatment of excess weight from improving willpower, character, and or a person’s ability to withstand the misery of starvation. Articles like this that challenge the conventional EBM thinking are fantastic tools by which to reach people wanting to understand the science.